
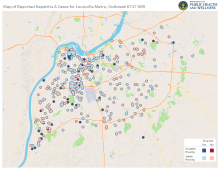
Photo: Louisville Metro Public Health And Wellness
The Louisville Metro Department of Public Health and Wellness is reminding residents to get immunized against hepatitis A and the flu.
“While we have seen some encouraging trends in Louisville with the number of new hepatitis A cases falling over the past six months, the hepatitis outbreak isn’t over yet,” said Dr. Sarah Moyer, director of the Metro Department of Public Health and Wellness and the city’s chief heath strategist. “In other areas of the state, new cases have grown quickly. In fact, nearly 80% of Kentucky counties have a hepatitis A outbreak. If you haven’t already done so, please get immunized against hepatitis A, especially considering all the travelling people do during the Thanksgiving holidays. Protect yourself and your family. Get immunized!”
“Also, please get a flu shot’” said Dr. Moyer. “Last year 49 people in Louisville died of the flu and its complications. So, when you’re out getting your hep A shot, get a flu shot as well.”
As the hepatitis A outbreak continues to spread throughout Kentucky and the surrounding region, new cases per day in Louisville fell for the sixth month in a row. New cases in Louisville have fallen from more than four per day in April to less than one per day in October. October’s new case per day rate of 0.58 was close to the same (0.39) as what it was in October 2017, before the outbreak was declared.
As of November 3, Kentucky had 2,545 hepatitis A cases and 17 deaths spread out over ninety-four counties. By comparison, Louisville had 634 cases (as of November 13) and five deaths. While Louisville once had the overwhelming majority of Kentucky’s hepatitis A cases, it now has less than 25% of the state’s cases.
More than 83,000 hepatitis A immunizations have been given across Louisville since the outbreak was declared, nearly 21,000 by Public Health and Wellness alone. The CDC has called Louisville’s response to the outbreak “the gold standard” for other cities to emulate.
Hepatitis A immunizations are widely available at local pharmacies and health care providers. The cost is covered by most insurance plans. People should check with their health insurance provider on where the insurer prefers that they go to get the vaccine and what, if any, cost might be associated with it.
For information on where to obtain the hepatitis A vaccine for those insured or uninsured, CLICK HERE.
 Kentucky’s current hepatitis A outbreak is now the biggest outbreak in the United States and the biggest ever recorded in both Kentucky and Louisville. As of July 7, the outbreak had struck 65 Kentucky counties with 1,094 hepatis A cases and 8 deaths. As of July 17, Louisville had 540 cases with 4 of the state’s 8 deaths. While the outbreak continues to grow and spread throughout the state, there is evidence that it may be declining in Louisvil
Kentucky’s current hepatitis A outbreak is now the biggest outbreak in the United States and the biggest ever recorded in both Kentucky and Louisville. As of July 7, the outbreak had struck 65 Kentucky counties with 1,094 hepatis A cases and 8 deaths. As of July 17, Louisville had 540 cases with 4 of the state’s 8 deaths. While the outbreak continues to grow and spread throughout the state, there is evidence that it may be declining in Louisvil
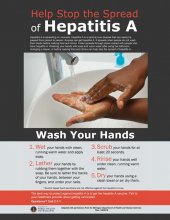
State and local officials urge everyone in Louisville and in any county in Kentucky that is part of the current hepatitis A outbreak to get immunized. They also remind everyone to practice good hand hygiene, particularly after using the restroom and before eating or preparing food.
New hepatitis cases per day have been trending downward in Louisville since April with 4.1 in April, 3.8 in May, 2.5 in June, and so far, 1.67 in July. “While there is evidence that new cases may be trending downward in Louisville,” said Dr. Sarah Moyer, director of the Louisville Metro Department of Public Health and Wellness, “this no time to get complacent. Anyone can get hepatitis A during this outbreak. It is being spread through person to person contact. The best ways to protect yourself and others are to get vaccinated and wash your hands often with soap and warm water.”
Health officials stressed that the virus in this outbreak is being passed person-to-person. There has been no evidence that it is being spread by food or drink as was the case during the hepatitis A outbreak that struck Louisville in 1988. The outbreak remains centered primarily among those who use illegal drugs and among the homeless; however, about 10% of cases do not fall into either of those group
“It’s been gratifying to see the Louisville Metro Department of Public Health and Wellness and local public health departments across the state coming together to combat the outbreak,” said Dr. Jeffrey Howard, commissioner of the Kentucky Department for Public Health. “Our surveillance and the fact that we’ve hospitalized about 60% of all cases has kept our death rate below that of other states experiencing hepatitis A outbreaks.”
In Louisville, 63% of the people (337 out 536) who were infected with hepatitis A have been hospitalized. Across the state, there have been eight deaths, including four in Louisville. The genetic fingerprint of the hepatitis A virus Louisville and in Kentucky matches outbreaks in San Diego California and Salt Lake City Utah.
“Louisville has done a superb job in rolling vaccine out to the homeless and the drug-using populations,” said Doug Thoroughman of the Centers for Disease Control and Prevention. “They are the gold standard of how to respond to an outbreak of this kind.”
More than 78,000 hepatitis A immunizations have been given locally in response to the current hepatitis A outbreak, more than 16,000 by the Department of Public Health and Wellness alone. Massive immunization and outreach efforts among the homeless in shelters, camps and at health facilities that serve the homeless in the early stages of the outbreak has limited the spread of hepatitis A among that population.
“I can’t overemphasize the importance of protecting yourself and others from hepatitis A by getting vaccinated,” said Dr. Moyer. “This vaccine is very well-tolerated. Most insurance plans cover the cost and there are ways those who are uninsured can get immunized for little to no cost. The outbreak will stop when most people living in Louisville are protected through vaccination.”
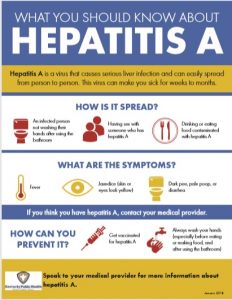
On November 21, 2017 the Kentucky Department for Public Health declared an outbreak of acute hepatitis A in multiple counties throughout the state. Hepatitis A is a vaccine-preventable, communicable disease of the liver caused by a virus. It is usually transmitted person-to-person through the fecal-oral route or consumption of contaminated food or water. Most adults with hepatitis A symptoms may experience fatigue, low appetite, stomach pain, nausea, or jaundice, that usually resolve within 2 months of infection; most children less than 6 years of age do not have symptoms or have an unrecognized infection. Antibodies produced in response to hepatitis A infection last for life and protect against reinfection. The best way to prevent hepatitis A infection is to get vaccinated.
Additional information and a list of places in Louisville to get vaccinated can be found at https://louisvilleky.gov/government/health-wellness/hepatitis or by calling 211.
 The number of people in Louisville who are getting hepatitis A continues to grow. As of today, there have been 478 cases and three deaths. Here are 10 key things to know:
The number of people in Louisville who are getting hepatitis A continues to grow. As of today, there have been 478 cases and three deaths. Here are 10 key things to know:
- The hepatitis A virus is being spread through person to person contact: Sharing a home, a cigarette, marijuana joint, a drink, or sex with someone who has the virus puts you at high risk.
- There have been cases of hepatitis A in every Louisville ZIP code.
- While the outbreak is largely centered in people who use drugs (any kind of drug use, not just injecting) and people who are homeless, 1 out of 8 cases report no risk factors.
- More than 60 percent of the 478 people who have had hepatitis A have been hospitalized. Getting hepatitis A can make you very sick.
- A person can have hepatitis A for up to 2 weeks before symptoms ever develop. During that 2 weeks they are contagious and exposing others to the virus.
- The hepatitis A virus can live for a long time on surfaces. Disinfecting kitchens and particularly any restroom open to public use with a solution of bleach and water is the most effective way to kill the virus. Specific disinfection guidelines can be found here.
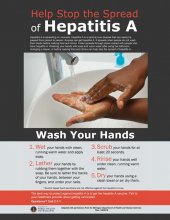
- Washing your hands thoroughly and often with warm water and soap is a way to protect yourself from many diseases, including hepatitis A. Be aware that hand sanitizer has not been proven as effective as handwashing against hepatitis A.
- For the best protection, you need to be vaccinated against hepatitis A. The Louisville Metro Department of Public Health and Wellness as well as the Kentucky Department for Public Health have been encouraging residents of Jefferson and any other counties with a hepatitis A outbreak to get vaccinated for several months. “Our hepatitis A outbreak will stop when the majority of our Louisville residents are vaccinated,” said Dr. Sarah Moyer, director, Louisville Metro Department of Public Health and Wellness.
- Most health insurance plans should cover 100 percent of the cost of the hepatitis A vaccination. If your pharmacist or healthcare provider tells you there’s a cost, contact your health insurance provider to find out where they allow you to get vaccinated at no cost.
- If you get diagnosed with hepatitis A and we call you, please talk to us. When someone gets infected with a communicable disease, a nurse or epidemiologist from Public Health and Wellness will contact them. Any information you share is protected and helps us make progress in stopping the spread of hepatitis A.
For more information about hepatitis A visit https://louisvilleky.gov/government/health-wellness/hepatitis or call 211.
 An employee of the White Castle restaurant at 2350 Greene Way has been diagnosed with acute hepatitis A.
An employee of the White Castle restaurant at 2350 Greene Way has been diagnosed with acute hepatitis A.
Customers who ate at this White Castle from May 29, 2018 to June 8, 2018 may have been exposed to the hepatitis A virus. While the risk of contracting hepatitis A from eating at this restaurant is low, the Louisville Metro Department of Public Health and Wellness is issuing this advisory out of an abundance of caution. The hepatitis A outbreak remains centered among who use illegal drugs and the homeless.
When a food service worker is diagnosed with hepatitis A, he or she is immediately excluded from work and not allowed to return without release from his or her medical provider. Additionally, all employees at the establishment are vaccinated and disinfection and sanitation practices are followed. This White Castle scored 95-A and 100-A and on its last two health inspections.
Symptoms of hepatitis A are fatigue, decreased appetite, stomach pain, nausea, darkened urine, pale stools and jaundice (yellowing of the skin and eyes). People can become ill 15 to 50 days after being exposed to the virus. Anyone experiencing symptoms should seek medical attention.
Hepatitis A is usually transmitted by putting something in your mouth such as an object, food or drink, which has been in contact with the feces of an infected person. In November, the Kentucky Department for Public Health declared a statewide hepatitis A outbreak and has recommended that all residents be vaccinated. Since the outbreak began there have been 457 cases diagnosed in Louisville and more than 75,000 vaccinated.
“Food-borne transmission has not been a factor in this outbreak,” said Dr. Lori Caloia, medical director of the Louisville Metro Department of Public Health and Wellness. “The virus continues to be transmitted person-to-person, primarily among those who use illegal drugs and the homeless. We have had a small number of food workers diagnosed with hepatitis A and the restaurant industry throughout Louisville continues to get their workers immunized. More than 5,800 local food service employees have been vaccinated against hepatitis A.”
Reduced-cost vaccinations continue to be available to restaurant workers. Restaurant workers wishing to be vaccinated should contact their managers for details.
The best ways to prevent hepatitis A infection are to get vaccinated and to practice good handwashing. “Washing your hands thoroughly and often with warm water and soap, especially before preparing meals or eating, after using the bathroom or changing a diaper is a proven way to prevent the spread of diseases,” Dr. Caloia added. “Hand sanitizer is not as effective as hand washing against hepatitis A.”
For more information about hepatitis A visit https://louisvilleky.gov/government/health-wellness/hepatitis or call 211.
 An employee of the Speedway located at 5400 Antle Dr. has been diagnosed with acute hepatitis A.
An employee of the Speedway located at 5400 Antle Dr. has been diagnosed with acute hepatitis A.
Only customers who ate prepared food products such as pizza, hot dogs, breakfast sandwiches at this Speedway from May 15, 2018 to May 31, 2018 may have been exposed to the hepatitis A virus. Customers who purchased fuel or packaged goods are not at risk.
While the risk of contracting hepatitis A from eating at Speedway is low, the Louisville Metro Department of Public Health and Wellness is issuing this advisory out of an abundance of caution. The hepatitis A outbreak remains centered among the homeless and those who use illegal drugs.
When a food service worker is diagnosed with hepatitis A, he or she is immediately excluded from work and not allowed to return without release from his or her medical provider. Additionally, all employees at the establishment are vaccinated and disinfection and sanitation practices are followed. This Speedway’s last two food service inspection scores were 98-A and 100-A.
Symptoms of hepatitis A are fatigue, decreased appetite, stomach pain, nausea, darkened urine, pale stools and jaundice (yellowing of the skin and eyes). People can become ill 15 to 50 days after being exposed to the virus. Anyone experiencing symptoms should seek medical attention.
Hepatitis A is usually transmitted by putting something in your mouth such as an object, food or drink, which has been in contact with the feces of an infected person. In November, the Kentucky Department for Public Health declared a statewide hepatitis A outbreak and has recommended that all residents be vaccinated. Since the outbreak began there have been 446 cases diagnosed in Louisville and almost 73,000 vaccinated. Of those, more than 5,700 are food workers.
“Food-borne transmission has not been a factor in this outbreak,” said Dr. Lori Caloia, medical director of the Louisville Metro Department of Public Health and Wellness. “The virus continues to be transmitted person-to-person, primarily among those who use illegal drugs and the homeless. We have had a very small number of food workers diagnosed with hepatitis A. We continue to encourage the restaurant industry to get their workers immunized.”
Reduced-cost vaccinations continue to be available to restaurant workers. Restaurant workers wishing to be vaccinated should contact their managers for details.
The best ways to prevent hepatitis A infection are to get vaccinated and to practice good handwashing. “Washing your hands thoroughly and often with warm water and soap, especially before preparing meals or eating, after using the bathroom or changing a diaper is a proven way to prevent the spread of diseases,” Dr. Caloia added. “Hand sanitizer is not as effective as hand washing against hepatitis A.”
For more information about hepatitis A visit https://louisvilleky.gov/government/health-wellness/hepatitis or call 211.
 An employee of Denny’s restaurant at 4030 Dutchman’s Lane in St. Matthews has been diagnosed with acute hepatitis A. Another employee at the same restaurant was diagnosed with acute hepatitis A in March. The two cases are not related.
An employee of Denny’s restaurant at 4030 Dutchman’s Lane in St. Matthews has been diagnosed with acute hepatitis A. Another employee at the same restaurant was diagnosed with acute hepatitis A in March. The two cases are not related.
Customers who ate at this Denny’s from May 4, 2018 to May 24, 2018 may have been exposed to the hepatitis A virus. While the risk of contracting hepatitis A from eating at this restaurant is low, the Louisville Metro Department of Public Health and Wellness is issuing this advisory out of an abundance of caution. The hepatitis A outbreak remains centered among the homeless and those who use illegal drugs.
When a food service worker is diagnosed with hepatitis A, he or she is immediately excluded from work and not allowed to return without release from his or her medical provider. Additionally, all employees at the establishment are vaccinated and disinfection and sanitation practices are followed. The St. Matthews Denny’s scored 93-A and 94-A on its last two health inspections.
Symptoms of hepatitis A are fatigue, decreased appetite, stomach pain, nausea, darkened urine, pale stools and jaundice (yellowing of the skin and eyes). People can become ill 15 to 50 days after being exposed to the virus. Anyone experiencing symptoms should seek medical attention.
Hepatitis A is usually transmitted by putting something in your mouth such as an object, food or drink, which has been in contact with the feces of an infected person. In November, the Kentucky Department for Public Health declared a statewide hepatitis A outbreak and has recommended that all residents be vaccinated. Since the outbreak began there have been 413 cases diagnosed in Louisville and more than 66,500 vaccinated.
“Food-borne transmission has not been a factor in this outbreak,” said Dr. Lori Caloia, medical director of the Louisville Metro Department of Public Health and Wellness. “The virus continues to be transmitted person-to-person, primarily among those who use illegal drugs and the homeless. We have had a very small number of food workers diagnosed with hepatitis A and the restaurant industry throughout Louisville continues to get their workers immunized. More than 5,700 local food service employees have been vaccinated against hepatitis A.”
Reduced-cost vaccinations continue to be available to restaurant workers. Restaurant workers wishing to be vaccinated should contact their managers for details.
The best ways to prevent hepatitis A infection are to get vaccinated and to practice good handwashing. “Washing your hands thoroughly and often with warm water and soap, especially before preparing meals or eating, after using the bathroom or changing a diaper is a proven way to prevent the spread of diseases,” Dr. Caloia added. “Hand sanitizer is not as effective as hand washing against hepatitis A.”
For more information about hepatitis A visit https://louisvilleky.gov/government/health-wellness/hepatitis or call 211.
 An employee of the Texas Roadhouse restaurant at 13321 Shelbyville Rd. has been diagnosed with acute hepatitis A.
An employee of the Texas Roadhouse restaurant at 13321 Shelbyville Rd. has been diagnosed with acute hepatitis A.
Customers who ate at this Texas Roadhouse from April 11, 2018 to April 25, 2018 may have been exposed to the hepatitis A virus. While the risk of contracting hepatitis A from eating at this restaurant is low, the Louisville Metro Department of Public Health and Wellness is issuing this advisory out of an abundance of caution. The hepatitis A outbreak remains centered among the homeless and those who use drugs.
When a food service worker is diagnosed with hepatitis A, he or she is immediately excluded from work and not allowed to return without release from his or her medical provider. Additionally, all employees at the establishment are vaccinated and disinfection and sanitation practices are followed. Texas Roadhouse scored 96-A and 97-A on its last two health inspections.
Symptoms of hepatitis A are fatigue, decreased appetite, stomach pain, nausea, darkened urine, pale stools and jaundice (yellowing of the skin and eyes). People can become ill 15 to 50 days after being exposed to the virus. Anyone experiencing symptoms should seek medical attention.
Hepatitis A is usually transmitted by putting something in your mouth such as an object, food or drink, which has been in contact with the feces of an infected person. In November, the Kentucky Department for Public Health declared a statewide hepatitis A outbreak. Since the outbreak began there have been 327 cases diagnosed in Louisville and nearly 27,000 vaccinated.
“While we have had a very small number of food workers diagnosed with hepatitis A in our community, there still has been NO foodborne transmission,” said Dr. Lori Caloia, medical director. “Also, our restaurant industry has really stepped up to the plate to get their workers immunized. About 5,000 local food service employees have been vaccinated against hepatitis A.”
The best ways to prevent hepatitis A infection are to get vaccinated and to practice good handwashing. “Washing your hands thoroughly and often with warm water and soap, especially before preparing meals or eating, after using the bathroom or changing a diaper is a proven way to prevent the spread of diseases,” Dr. Caloia added. “Hand sanitizer is not as effective as hand washing against hepatitis A.”
For more information about hepatitis A visit https://louisvilleky.gov/government/health-wellness/hepatitis or call 211.
 Weather
Weather Traffic
Traffic @LouisvilleDispatch
@LouisvilleDispatch @LouisvilleDisp
@LouisvilleDisp Subscribe
Subscribe