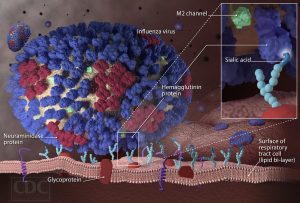
 The Department for Public Health (DPH), within the Cabinet for Health and Family Services, is reminding Kentuckians to get vaccinated against the flu.
The Department for Public Health (DPH), within the Cabinet for Health and Family Services, is reminding Kentuckians to get vaccinated against the flu.
“Getting the flu can be debilitating and sometimes life-threatening,” said Jeffrey Howard, M.D., commissioner of DPH. “Vaccination is the best tool we have to prevent the flu and it is also extremely important to take simple preventive steps to avoid the flu and other illnesses that tend to circulate at this time of year – wash your hands frequently, cover your mouth when you cough or sneeze and stay home when you’re sick.”
DPH officials report weekly influenza activity to the CDC as part of statewide flu surveillance efforts. The weekly report is located online at https://healthalerts.ky.gov/Pages/FluActivity.aspx will be updated by noon each Friday. Kentucky currently is reporting 28 laboratory-confirmed cases of flu and one influenza-related death. The state flu activity level is currently classified as “sporadic”. The report consists of laboratory-confirmed cases of influenza that are defined by molecular virus testing and positive virus culture test results. Rapid positive influenza tests are not included in this report, but are used as an indicator of flu-like illness circulating across the state.
The Centers for Disease Control and Prevention (CDC) Advisory Committee on Immunization Practices (ACIP) recommends flu vaccine for all individuals six months of age and older. People who are strongly encouraged to receive the flu vaccine because they may be at higher risk for complications or negative consequences include:
- Children age six months through 59 months;
- Women who are or will be pregnant during the influenza season;
- Persons 50 years of age or older;
- Persons with extreme obesity (Body Mass Index of 40 or greater);
- Persons aged six months and older with chronic health problems;
- Residents of nursing homes and other long-term care facilities;
- Household contacts (including children) and caregivers of children aged ≤59 months
- Household contacts and caregivers or people who live with a person at high-risk for
complications from the flu; and - Health care workers, including physicians, nurses, and other workers in inpatient and outpatient-care settings, medical emergency-response workers (e.g., paramedics and emergency medical technicians), employees of nursing home and long-term care facilities who have contact with patients or residents, and students in these professions who will have contact with patients.
Adequate supplies of flu vaccine are expected to be available for this year’s flu season. Vaccination can be given any time during the flu season, but providers are encouraged to administer the vaccine as soon as possible.
During the 2016-17 and 2017-18 influenza seasons, ACIP recommended that Flu Mist not be used because of concerns about low effectiveness against influenza A (H1N1). However, ACIP recommends that FluMist once again be an option for vaccination during the 2018-2019 influenza season for persons for whom it is age-appropriate and who have no medical contraindications. The change in recommendation is a result of the influenza A (H1N1) strain being changed in the current FluMist formulation.
Due to the timing of the decision by the ACIP regarding use of FluMist, the Kentucky Vaccines for Children Program (VFC) will not be offering FluMist for VFC or KCHIP patients during the 2018-2019 influenza season. However, some private providers will offer FluMist this season for their patients.
The flu vaccine is especially important in light of the severe season experienced last year across the U.S. The CDC reports that more than 900,000 flu-related hospitalizations occurred and more than 80,000 people died as a result of flu. In Kentucky there were 333 flu-related deaths, 5 of which were pediatric. Of the pediatric flu deaths reported in last year’s season, more than one-third of these occurred among healthy children between the ages of 6 months and 4 years.
It is especially important for pregnant women to be vaccinated before or during pregnancy. Antibodies cross the placenta and provide immunity to infants up to 6 months of age, when the infant is eligible to receive their dose of flu vaccine.
DPH relies on sites such as doctors’ offices, hospitals and health departments to help track the level of influenza activity in the state and to identify which strains of the flu are circulating in Kentucky. These voluntary sites collect data and report influenza-like illness (ILI) cases according to age groups each week. This sampling represents only a small percentage of influenza cases for the state, but contributes to the ongoing assessment of flu activity in the Commonwealth and helps determine the weekly level of flu activity.
Infection with the flu virus can cause fever, headache, cough, sore throat, runny nose, sneezing and body aches. Flu can be very contagious. For more information on influenza or the availability of flu vaccine, Kentuckians should contact their primary care medical provider or local health department. Influenza information is also available online at https://www.cdc.gov/flu/index.htm.
 As part of “No Shave November,” the Kentucky Department for Public Health (DPH) within the Cabinet for Health and Family Services is emphasizing the importance of colon cancer awareness and prevention. The effort is part of the ongoing 52 Weeks of Public Health Campaign.
As part of “No Shave November,” the Kentucky Department for Public Health (DPH) within the Cabinet for Health and Family Services is emphasizing the importance of colon cancer awareness and prevention. The effort is part of the ongoing 52 Weeks of Public Health Campaign.
Colon cancer remains the second leading cause of cancer deaths in the U.S. despite being considered the most easily preventable cancer. Screening and early diagnosis are important for long-term survival, along with healthy lifestyle habits including a healthy diet, regular exercise and avoiding smoking and other forms of tobacco.
“Although screening is the best way to decrease the risk of colon cancer, improving your overall health with a few healthy living style choices will decrease your chances of developing colon cancer,” said Dr. Jeffrey D. Howard, acting DPH commissioner.
Colon cancers often develop from precancerous polyps (abnormal growths) in the colon or rectum. Detection of the pre-cancerous polyps can be found through screenings such as colonoscopy, sigmoidoscopy, barium enema or virtual colonoscopy. Screenings for colon cancer should be done on men and women starting at 45 to 50 years of age and thereafter as deemed necessary by your health care provider and screening results.
Early signs and symptoms of colon may include:
- Rectal bleeding
- Change in bowel movement frequency
- Change in stool size
- Unexplained anemia (low red blood cells)
- Unexplained weight loss
- Frequent abdominal pain
- Constant tiredness
- Vomiting
To learn about how you can get screened for colon cancer, visit the Kentucky Colon Cancer Screening Program website.
 The Kentucky Department for Public Health (DPH) has declared an outbreak of acute hepatitis A with cases in multiple counties in Kentucky.
The Kentucky Department for Public Health (DPH) has declared an outbreak of acute hepatitis A with cases in multiple counties in Kentucky.
In total, 31 cases of acute (rapid onset with symptoms of illness) Hepatitis A have been reported throughout Kentucky in 2017, a 50 percent increase above the average of 20 cases per year reported over the past 10 years. Jefferson County has had 19 confirmed cases, most of which have occurred since August. Cases have been reported in Jefferson, Shelby, Bullitt, Hardin, Henry, Anderson, Mason, Christian, Madison, Fayette, McCracken, Hopkins, and Leslie counties.
DPH, the Louisville Metro Department of Public Health and Wellness (LMPHW), and other health departments have been working to stop the spread of Hepatitis A in the region. Common risk factors of homelessness or drug use have been identified among 12 of the cases in Jefferson County. No deaths have been attributed to this outbreak.
“Acute hepatitis A is a serious and potentially life-threatening infectious disease,” said Dr. Jonathan Ballard, State Epidemiologist for KDPH. “We are working to identify anyone who has been exposed to cases associated with this outbreak and urging those experiencing symptoms of the illness to contact their healthcare provider for appropriate evaluation and medical treatment, if necessary.”
Public Health staff have conducted enhanced surveillance for acute hepatitis A cases, investigated each new case in a county to identify risk factors and close contacts, and recommended postexposure prophylaxis for susceptible close contacts. In addition, laboratory specimens from recently diagnosed cases have been sent for specialized genetic testing of the hepatitis A virus at the Centers of Disease Control and Prevention (CDC) in Atlanta.
Thus far test results match the genotype associated with an acute Hepatitis A outbreaks in California.
“Hepatitis A is a vaccine-preventable illness. All children, aged 1 year through 18 years, are recommended to get the Hepatitis A vaccine as well as adults with increased risk factors or certain medical conditions,” said Dr. Ballard. “DPH is working with the LMPHW and other local health departments to develop an emergency vaccine distribution plan for the area most impacted by the outbreak.”
Increased risk factors include homelessness; all forms of substance use disorder; people with direct contact with someone who has Hepatitis A; travelers to countries where hepatitis A is common; men who have sexual contact with men; household members or caregivers of a recent adoptee from countries where hepatitis A is common; people with clotting factor disorders, such as hemophilia.
In addition, DPH is activating the State Health Operations Center (SHOC) to Level 3 to help coordinate the public health response.
Other than age-appropriate vaccinations, the best way to keep from getting Hepatitis A is to wash your hands using warm water and soap, to handle uncooked food appropriately and to fully cook food. Always wash your hands before touching or eating food, after using the toilet and after changing a diaper. When soap and water are not available, use alcohol-based disposable hand wipes or gel sanitizers.
Signs and symptoms of Hepatitis A include jaundice (yellowing of the skin or eyes), dark-colored urine, fatigue, abdominal pain, loss of appetite, nausea, diarrhea and fever. The virus is found in the stool of people infected with Hepatitis A and is usually spread from person to person by putting something in the mouth (even though it might look clean) that has been contaminated with the stool of a person infected with Hepatitis A. It is often transmitted when people do not wash their hands properly or by eating uncooked or undercooked food.
Not everyone with the acute Hepatitis A virus infection will develop symptoms, however, if symptoms do develop, they may include fever, jaundice or yellowing of the skin, vomiting, fatigue, and grey-colored stools. Persons with symptoms should seek medical care for prompt diagnosis and treatment.
Additional information about Hepatitis A is available from the CDC.
 Frying a turkey can be a fun and tasty alternative to the traditional baked dishes of the holidays. As many start to plan menus, the Department for Public Health (DPH), within the Cabinet for Health and Family Services (CHFS), wants to remind Kentuckians that fryers – multi-use kettles used for deep frying foods – also can be dangerous when not handled with care. The safety promotion is part of DPH’s ongoing 52 Weeks of Public Health Campaign.
Frying a turkey can be a fun and tasty alternative to the traditional baked dishes of the holidays. As many start to plan menus, the Department for Public Health (DPH), within the Cabinet for Health and Family Services (CHFS), wants to remind Kentuckians that fryers – multi-use kettles used for deep frying foods – also can be dangerous when not handled with care. The safety promotion is part of DPH’s ongoing 52 Weeks of Public Health Campaign.
Since 2002, the Consumer Product Safety Commission (CPSC) has tracked more than 168 turkey-fryer related fire, burn, explosion or CO poisoning incidents, including 672 injuries and $8 million in property damage. Hazard scenarios have varied from house fires, ignition of oil used in the fryers themselves, and burn-causing oil splashes.
“Turkey fryers have steadily grown in popularity over the past two decades, but they pose some risk if not used properly,” said Dr. Jeffrey Howard, acting commissioner for DPH. “By following a few guidelines and using precaution, adverse circumstances can be avoided. We want all Kentuckians to have a happy and safe holiday season and we ask that everyone follow some simple safety guidelines when cooking – or frying – your holiday food.”
According to the CPSC, the majority of reported turkey fryer incidents occurred while the oil was being heated, prior to adding turkey. For this reason, it is very important that consumers monitor the temperature of oil closely. If any smoke at all is noticed coming from heating a pot of oil, the burner should be turned off immediately because the oil is overheated.
Consumers who choose to fry turkeys always should remember to keep the fryer in full view while the burner is on and to place the fryer in open area away from walls, fences or other structures. Fryers should be stored outside and never used under a garage, breezeway, carport or any other structure that can catch fire.
To avoid burns, food should be raised and lowered slowly and bare skin should be covered. It’s also important to check the oil temperature frequently. If the oil should begin to smoke, the gas supply should be turned off immediately.
If a fire occurs, immediately call 911. Do not attempt to extinguish fire with water.
Here’s a look at the best way to avoid accidents or injuries from turkey fryers this holiday season:
- Make sure there is at least two feet of space between the propane tank and fryer burner.
- Place the gas tank and fryer so that wind blows heat of the fryer away from tank.
- Center the pot over the burner on the cooker.
- Completely thaw (USDA says 24 hours for every four to five pounds) and dry turkey before cooking. Partially frozen and/or wet turkeys can produce excessive hot oil splatter when added to the oil.
Follow the manufacturer’s instructions to determine the proper amount of oil to add. If those are not available:
- Place turkey in pot.
- Fill with water until the turkey is covered by about one-half inch of water.
- Remove and dry turkey.
- Mark the water level. Dump water, dry the pot, and fill with oil to the marked level.
 As part of the 52 Weeks of Public Health campaign, the Department for Public Health, located within the Cabinet for Health and Family Services (CHFS), urges the public to take steps to avoid injury and illness during periods of extreme summertime heat, particularly dangers associated with leaving children in vehicles.
As part of the 52 Weeks of Public Health campaign, the Department for Public Health, located within the Cabinet for Health and Family Services (CHFS), urges the public to take steps to avoid injury and illness during periods of extreme summertime heat, particularly dangers associated with leaving children in vehicles.
“Extreme temperatures are cause for concern, so we advise the public to take necessary steps to keep cool and prevent harm,” said Hiram C. Polk Jr., MD, DPH commissioner. “Serious injury – particularly for children exposed to extreme levels of heat – can occur. Everyone should take steps to avoid these dangers.”
According to Kids and Cars, an organization that works to raise awareness of the dangers of leaving children in hot vehicles, 39 children died last year due to heatstroke – medically termed “hyperthermia”.
“We want all our citizens to understand the dangers of extreme heat, particularly the danger of leaving children in hot cars,” continued Dr. Polk. “Not only are extreme temperatures uncomfortable, they also present a significant health danger. This is particularly true for vulnerable populations such as young children and the elderly.”
Several measures are recommended to prevent these types of deaths from occurring. They include:
- Create reminders. More than half of child heat stroke deaths occur because parents and caregivers become distracted and exit their vehicle without their child. To help prevent these tragedies parents can:
- Place a cell phone, PDA, purse, briefcase, gym bag or something that is needed at your next stop on the floor in front of a child in a backseat. This will help you see your child when you open the rear door and reach for your belongings.
- Set the alarm on your cell phone as a reminder to you to drop your child off at day care.
- Set your computer calendar program to ask, “Did you drop off at day care today?”
- Establish a plan with your day care that if your child fails to arrive within an agreed upon time, you will be called. Be especially mindful of your child if you change your routine for day care.
- Don’t underestimate the risk. The inside of vehicles can quickly heat up, even on relatively cool days, so you should never leave your child alone in a car. Don’t underestimate the risks and leave them even “just for a minute.”
- Lock cars and trucks. Thirty percent of the recorded heat stroke deaths in the U.S. occur because a child was playing in an unattended vehicle. These deaths can be prevented by simply locking the vehicle doors to help assure that kids don’t enter the vehicles and become trapped.
- Immediately dial 911 if you see an unattended child in a car. EMS professionals are trained to determine if a child is in trouble. The body temperature of children rises three to five times faster than adults. As a result, children are much more vulnerable to heat stroke. Check vehicles and trunks first if a child is missing.
Additional tips are recommended to avoid other heat-related injury and illness:
- Drink plenty of fluids. Increase your normal fluid intake regardless of your activity level. You will need to drink more fluids than your thirst level indicates. This is especially true for people age 65 or older who often have a decreased ability to respond to external temperature changes. In addition, avoid drinking beverages containing alcohol, because they will actually cause you to lose more fluid.
- Wear appropriate clothing and sunscreen. Choose lightweight, light colored, loose fitting clothing. In the hot sun, wear a wide-brimmed hat that will provide shade and keep the head cool. Sunscreen should be SPF 15 or greater and applied 30 minutes before going out into the sun.
- Stay cool indoors. The most efficient way to beat the heat is to stay in an air-conditioned area. If you do not have an air conditioner, consider visiting a mall or public library.
- Schedule outdoor activities carefully. If you must be out in the heat, try to plan your activities so that you are outdoors either before noon or in the evening. Rest periodically so your body’s thermostat will have a chance to recover.
- Use a buddy system. When working in the heat, monitor the condition of your co-workers and have someone do the same for you. Heat-induced illness can cause a person to become confused or lose consciousness.
- Monitor those at high risk. Those at greatest risk of heat-related illness include:
- Infants and children up to 4 years of age
- People 65 years of age or older
- People who are overweight
- People who overexert during work or exercise
- People who are ill or on certain medications for blood pressure or diuretics

Photo: CHFS
As part of the 52 Weeks of Public Health campaign, the Kentucky Department for Public Health (DPH), within the Cabinet for Health and Family Services (CHFS), along with local health departments across the state, is reminding the public about the potential for rabies exposure from contact with infected wildlife.
Wildlife rabies cases, primarily in bats, raccoons, skunks and foxes, have been identified in the U.S., and these result in human and animal exposures requiring thousands of human rabies post-exposure treatments and animal euthanasia or quarantines.
“Rabies is relatively rare in the U.S., but a dangerous, and often life-threatening condition, if contracted,” said Kelly Giesbrecht, state veterinarian with DPH. “We want to highlight the importance of rabies prevention and control efforts in our communities, while also reminding Kentuckians of the existing dangers of coming into contact with rabid wildlife. They should not be handled or treated as pets to avoid possible rabies exposure.”
Rabies, a viral disease of humans, pets and wild animals, is transmitted from animals to humans by the saliva of a rabid animal, usually from a bite. State law requires that all dogs, cats and ferrets maintain a current rabies vaccination. In Kentucky, there have been no human rabies cases from exposure to a rabid dog since dog vaccination became required by law in 1954. For more information about rabies, visit the DPH website at http://www.chfs.ky.gov/dph/epi/rabies.htm.
“We want the public to understand that rabies is still a serious public health concern, and we need to do everything we can to prevent it,” said Dr. Giesbrecht. “It is extremely important that we vaccinate all dogs, cats and ferrets in order to maintain this invisible barrier between rabid wildlife and humans.”
Contact bites from bats are the most common source of rabies exposure to humans in the United States. To minimize the risk for contracting rabies, it is best never to handle any bat. To prevent bats from entering your home, carefully examine your home for holes that might allow bats to enter the residence. Any openings larger than a quarter-inch by a half-inch could allow for bat entry. These openings should be blocked either with stainless steel wool or caulking in the fall or winter so you do not unintentionally trap bats within your home. Common ways for bats to enter homes include down the chimney, through openings around the chimney, through vents, through openings behind shutters, under doors, under siding, under eaves and under shingles.
There is no known medical cure for rabies once clinical symptoms are present. Symptoms include strange sensations at the site of the bite from a rabid animal, hallucinations and fear of water, all of which are quickly followed by death.
It is estimated that more than 59,000 people around the world die from rabies each year. Worldwide, more people die from rabies than from polio, diphtheria and yellow fever combined.
 Weather
Weather Traffic
Traffic @LouisvilleDispatch
@LouisvilleDispatch @LouisvilleDisp
@LouisvilleDisp Subscribe
Subscribe