 An employee of the Mark’s Feed Store restaurant at 11422 Shelbyville Rd. and an employee of Panera restaurant at 1801 Rudy Ln. have been diagnosed with acute hepatitis A.
An employee of the Mark’s Feed Store restaurant at 11422 Shelbyville Rd. and an employee of Panera restaurant at 1801 Rudy Ln. have been diagnosed with acute hepatitis A.
Customers who ate at Mark’s Feed Store from April 13 to April 27, 2018 and customers who ate at Panera from April 12 to April 28 may have been exposed to the hepatitis A virus. While the risk of contracting hepatitis A from having eaten at either of these restaurants is low, the Louisville Metro Department of Public Health and Wellness is issuing this advisory out of an abundance of caution. The hepatitis A outbreak remains centered among the homeless and those who use drugs.
When a food service worker is diagnosed with hepatitis A, he or she is immediately excluded from work and not allowed to return without release from his or her medical provider. Additionally, all employees at the establishment are vaccinated and disinfection and sanitation practices are followed.
Symptoms of hepatitis A are fatigue, decreased appetite, stomach pain, nausea, darkened urine, pale stools and jaundice (yellowing of the skin and eyes). People can become ill 15 to 50 days after being exposed to the virus. Anyone experiencing symptoms should seek medical attention.
Hepatitis A is usually transmitted by putting something in your mouth such as an object, food or drink, which has been in contact with the feces of an infected person. In November, the Kentucky Department for Public Health declared a statewide hepatitis A outbreak. Since the outbreak began there have been 304 cases diagnosed in Louisville and at least 26,662 vaccinated.
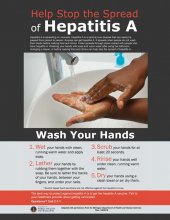
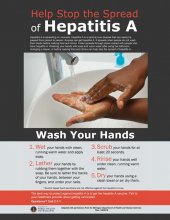
“The best ways to prevent hepatitis A infection are to get vaccinated and to practice good handwashing,” said Dr. Lori Caloia, medical director. “Washing your hands thoroughly and often with warm water and soap, especially before preparing meals or eating, after using the bathroom or changing a diaper is a proven way to prevent the spread of diseases. Hand sanitizer is not as effective as hand washing against hepatitis A.”
For more information about hepatitis A visit https://louisvilleky.gov/government/health-wellness/hepatitis or call 211.
 An employee of Bearno’s Pizza restaurant located at 9222 Westport Rd. has been diagnosed with acute hepatitis A. As a result, customers who ate at the restaurant from April 8 to April 22, 2018 may have been exposed to the hepatitis A virus.
An employee of Bearno’s Pizza restaurant located at 9222 Westport Rd. has been diagnosed with acute hepatitis A. As a result, customers who ate at the restaurant from April 8 to April 22, 2018 may have been exposed to the hepatitis A virus.
Symptoms of hepatitis A are fatigue, decreased appetite, stomach pain, nausea, darkened urine, pale stools and jaundice (yellowing of the skin and eyes). People can become ill 15 to 50 days after being exposed to the virus. Anyone experiencing symptoms should seek medical attention.
Hepatitis A is usually transmitted by putting something in your mouth such as an object, food or drink, which has been in contact with the feces of an infected person. In November, the Kentucky Department for Public Health declared a statewide hepatitis A outbreak. Since the outbreak began there have been 294 cases diagnosed in Louisville and more than 16,000 vaccinated.
“The best ways to prevent hepatitis A infection are to get vaccinated and to practice good handwashing,” said Dr. Lori Caloia, medical director. “Washing your hands thoroughly and often with warm water and soap, especially before preparing meals or eating, after using the bathroom or changing a diaper is a proven way to prevent the spread of diseases. Hand sanitizer is not as effective as hand washing against hepatitis A.”
For more information about hepatitis A visit https://louisvilleky.gov/government/health-wellness/hepatitis or call 211.

Photo: Louisville Metro Public Health And Wellness
An employee of the White Castle restaurant located at 3701 Seventh St. Rd. has been diagnosed with acute hepatitis A. As a result, customers who ate at the restaurant from April 6 to April 20, 2018 may have been exposed to the hepatitis A virus.
Symptoms of hepatitis A are fatigue, decreased appetite, stomach pain, nausea, darkened urine, pale stools and jaundice (yellowing of the skin and eyes). People can become ill 15 to 50 days after being exposed to the virus. Anyone experiencing symptoms should seek medical attention.
Hepatitis A is usually transmitted by putting something in your mouth such as an object, food or drink, which has been in contact with the feces of an infected person. In November, the Kentucky Department for Public Health declared a statewide hepatitis A outbreak. Since the outbreak began there have been 281 cases diagnosed in Louisville and more than 14,000 vaccinated.
“The best ways to prevent hepatitis A infection are to get vaccinated and to practice good handwashing,” said Dr. Lori Caloia, medical director. “Washing your hands thoroughly and often with warm water and soap, especially before preparing meals or eating, after using the bathroom or changing a diaper is a proven way to prevent the spread of diseases. Hand sanitizer is not as effective as hand washing against hepatitis A.”
The Department of Public Health and Wellness recommends anyone working in the hospitality industry, particularly those who serve or prepare food and beverages, protect themselves and others by getting the hepatitis A vaccine. White Castle will provide free hepatitis A vaccinations for their employees in the Louisville Metro area.
The department and the University of Louisville Global Health Center have partnered to offer below-cost vaccinations to all hospitality workers. The cost of the hepatitis A vaccine has been reduced from $65 to $25. Businesses with more than 20 employees can have a nurse come to their site to provide the immunizations. Businesses with fewer than 20 employees may designate vaccine for their employees to be immunized at U of L’s walk-in clinic. To arrange these employee immunizations, contact Dr. Ruth Carrico at 502-852-1324.
To date more than 50 local food service establishments have chosen to provide their employees the hepatitis A vaccine through this effort.
For more information about hepatitis A visit https://louisvilleky.gov/government/health-wellness/hepatitis or call 211.

Photo: Cabinet for Health and Family Services
Due to an ongoing outbreak of Hepatitis A, the Department for Public Health (DPH) within the Cabinet for Health and Family Services (CHFS), is recommending vaccination for everyone residing in Jefferson, Bullitt, Hardin, Greenup, Carter and Boyd counties.
To date, 214 cases have been reported in the Jefferson County/Louisville area. Bullitt, Hardin, Greenup, Carter and Boyd counties have each reported 5 or more cases for a total 311 cases associated with the outbreak. One death has been reported.
“Hepatitis A is a vaccine-preventable illness. DPH recommends all children, ages 1 year through 18, receive the Hepatitis A vaccine as well as adults who want to protect themselves from an acute hepatitis A infection,” said Dr. Jeffrey Howard, acting DPH commissioner. “In these counties with local transmission of the hepatitis A virus, we recommend everyone be vaccinated per guidelines to help stop this outbreak.”
For adults, the hepatitis A vaccine is typically given in two doses — an initial vaccination followed by another shot six months later. DPH recommends that all people in outbreak counties consult with their primary care doctor or insurance carrier regarding an in-network provider for administration of the hepatitis A vaccine. The Center for Disease and Control (CDC) recommends vaccination for people who wish to be protected against hepatitis A infection. For insured people, the hepatitis A vaccine should not require any out-of-pocket costs as long as policies are compliant with the federal Affordable Care Act.
Since 2006, the CDC has recommended children receive the hepatitis A vaccine series. Effective July 1, 2018, all Kentucky students in kindergarten through 12th grade must receive two doses of the Hepatitis A vaccine to attend school or receive a provisional certificate of immunization (unless their parents claim an exemption).
Signs and symptoms of Hepatitis A include jaundice (yellowing of the skin or eyes), dark-colored urine, fatigue, abdominal pain, loss of appetite, nausea, diarrhea and fever. The virus is found in the stool of people infected with Hepatitis A and typically spread from person to person contact. The disease often is transmitted when people do not wash their hands properly or do not have access to proper sanitation. DPH recommends individuals wash their hands often and particularly after using the restroom or before consuming food. Hand sanitizer should be used only when soap and water is unavailable.
While the current hepatitis A outbreak is occurring primarily within specific at-risk populations, including people who use illicit drugs (both injection and non-injection) and the homeless, through person-to-person transmission. Approximately, 30 percent of cases do not report any risk factors. Therefore, it is recommended that children and adults in counties with local transmission of the virus as part of this outbreak receive the hepatitis A vaccine.
Hepatitis A vaccine is widely available at local pharmacies and health care providers. For additional information on the hepatitis A vaccination, please visit https://www.cdc.gov/hepatitis/hav/afaq.htm#E1.

Photo: Louisville Metro Public Health And Wellness
The Louisville Metro Department of Public Health and Wellness continues to work to control an outbreak of acute hepatitis A that has centered in the city’s homeless and among those who use illicit drugs.
On November 21, 2017 the Kentucky Department for Public Health declared an outbreak of acute hepatitis A in several counties throughout the state. To date there have been 142 cases in Kentucky of which 124 have occurred Louisville. Today, the Kentucky Department of Public Health announced the death of a Jefferson County resident with multiple other health issues whose symptoms and lab results met the case definition of acute hepatitis A infection. This is the first death in Kentucky associated with this outbreak.
Hepatitis A is a vaccine-preventable, communicable disease of the liver caused by a virus. It is usually transmitted person-to-person through the fecal-oral route or consumption of contaminated food or water. Most adults with hepatitis A symptoms may experience fatigue, low appetite, stomach pain, nausea, or jaundice, that usually resolve within 2 months of infection; most children less than 6 years of age do not have symptoms or have an unrecognized infection. Antibodies produced in response to hepatitis A infection last for life and protect against reinfection. The best way to prevent hepatitis A infection is to get vaccinated.
Since the outbreak was declared in 2017, the Louisville Metro Department of Public Health and Wellness has activated its Incident Command System to coordinate its response to control the outbreak. The department has given nearly 6,000 hepatitis A immunizations at homeless shelters, homeless camps, recovery houses and at agencies such as Family Health Centers’ Phoenix Health Center. It has also provided immunizations at Metro Corrections, both at intake and in the general population. It regularly continues to provide immunizations at its syringe exchange sites, its Specialty Clinic and at the MORE Center.
In addition, the U of L pharmacy has provided immunizations for first responders at agencies such as EMS, Public Works and Louisville Fire. The Department of Public Health and Wellness is also working with Kroger Little Clinics and Walgreen’s to immunize other first responders. The Centers for Disease Control and Prevention (CDC) has praised Louisville’s response to the hepatitis A outbreak calling it the “gold standard” and a model for other cities to emulate.
“The best way to prevent hepatitis A is to get immunized,” said Dr. Lori Caloia, medical director of the Department of Public Health and Wellness. “Certainly those who have hepatitis B or C or who have other types of liver disease should get immunized,” she said. “Among these people hepatitis A can be fatal.”
“Almost everyone knows someone who uses drugs. People who use drugs should be encouraged to get immunized. Those who are homeless and those who work with the homeless should also get vaccinated,” said Dr. Caloia. “Anyone who wants to avoid getting hepatitis A should consult their health care provider to see if a hepatitis A immunization is right for them,” said Dr. Caloia.
To control the outbreak the Department of Public Health and Wellness is working with the Centers for Disease Control and Prevention to give free hepatitis A vaccinations to the homeless, those who work with the homeless and those who use illicit drugs. These groups can get free immunizations at the following times and locations.
- Louisville Metro Syringe Exchange
400 E. Gray St.
Mondays & Fridays 11am – 4pm
Tuesday & Wednesday 1pm – 6pm
Thursday 3pm – 6pm
Saturday 11am – 2pm - Family Health Center – Phoenix
712 E. Muhammad Ali Blvd.
Monday – Friday
8am – 4:30 pm
All others wishing hepatitis A vaccination should contact their healthcare provider or contact their local Kroger Little Clinic or Walgreen’s.
The Centers for Disease Control and Prevention recommends hepatitis A vaccination as follows:
- All children at age 1 year,
- Persons who are at increased risk for infection,
- Persons who are at increased risk for complications from hepatitis A, and
- Any person wishing to obtain immunity (protection).
Kentucky also now requires all schoolchildren in kindergarten through twelfth grade to get two doses of hepatitis A vaccine.
While the current hepatitis A outbreak in Louisville has centered in the homeless and those who use illicit drugs, the CDC also lists these groups as being at increased risk for hepatitis A.
Persons traveling to or working in countries that have high or intermediate endemicity of hepatitis A. Persons who travel to developing countries are at high risk for hepatitis A, even those traveling to urban areas, staying in luxury hotels, and those who report maintaining good hand hygiene and being careful about what they drink and eat (see https://wwwnc.cdc.gov/travel/yellowbook/2018/infectious-diseases-related-to-travel/hepatitis-a for more information).
Men who have sex with men. Men who have sex with men should be vaccinated.
Users of injection and non-injection drugs. Persons who use injection and non-injection drugs should be vaccinated.
Persons who have occupational risk for infection. Persons who work with HAV-infected primates or with HAV in a research laboratory setting should be vaccinated. No other groups have been shown to be at increased risk for HAV infection because of occupational exposure.
Persons who have chronic liver disease. Persons with chronic liver disease who have never had hepatitis A should be vaccinated, as they have a higher likelihood of having fulminant hepatitis A (i.e., rapid onset of liver failure, often leading to death). Persons who are either awaiting or have received liver transplants also should be vaccinated.
Persons who have clotting-factor disorders. Persons who have never had hepatitis A and who are administered clotting-factor concentrates, especially solvent detergent-treated preparations, should be vaccinated.
Household members and other close personal contacts of adopted children newly arriving from countries with high or intermediate hepatitis A endemicity. Previously unvaccinated persons who anticipate close personal contact (e.g., household contact or regular babysitting) with an international adoptee from a country of high or intermediate endemicity during the first 60 days following arrival of the adoptee in the United States should be vaccinated. The first dose of the 2-dose hepatitis A vaccine series should be administered as soon as adoption is planned, ideally 2 or more weeks before the arrival of the adoptee. More information is available at: https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5836a4.htm.
Persons with direct contact with persons who have hepatitis A. Persons who have been recently exposed to HAV and who have not previously received hepatitis A vaccine should be vaccinated. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5641a3.htm
Other than vaccination, the best way to keep from getting hepatitis A is to wash your hands using warm water and soap, to handle uncooked food appropriately, and to fully cook food. Always wash your hands before touching or eating food, after using the toilet, and after changing a diaper.
 Weather
Weather Traffic
Traffic @LouisvilleDispatch
@LouisvilleDispatch @LouisvilleDisp
@LouisvilleDisp Subscribe
Subscribe